What we know about the coronavirus: Symptoms, transmission and response. Information shared by Washignton Post for wider circulation.
Uh, oh. You wake up feeling crummy. Your throat hurts; maybe you have a cough. You are definitely anxious. What should you do? Can you get tested to rule out the novel coronavirus?
First, what’s wrong with me?
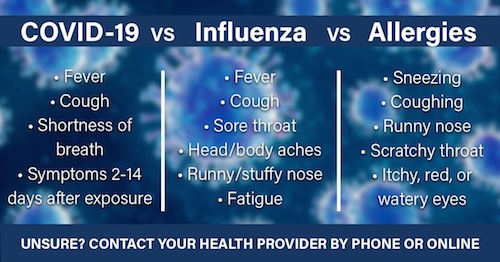
There’s a good chance it’s not Covid-19. You may have the flu, especially if you have aches and pains, or a bad cold. “A runny nose and itchy eyes — that’s not a problem,” said Gregory Poland, an infectious disease expert at the Mayo Clinic in Rochester, Minn.
But a high fever, a persistent cough — or signs of respiratory distress such as shortness of breath — means you could have the disease caused by the virus. For doctors trying to make diagnoses, context is key, Poland said. “Am I looking at a 12-year-old kid from a little town in Kansas with no cases or an 80-year-old with a chronic disease in New York City who just got off a cruise ship?”
So what if I think I might be infected?
Consult with your primary care doctor, if you have one. Don’t go to the doctor’s office or the emergency room without calling ahead. The coronavirus is highly contagious, and doctors want to protect themselves and their other patients from infection.
“We cannot have covid in the office,” said one Washington-area primary care physician who spoke on the condition of anonymity to protect patients’ privacy. “Our job is to keep people out of the hospital!” The doctor noted that her waiting room is frequently full of older patients with heart disease, cancer and other conditions for whom the coronavirus could be fatal.
Your doctor will assess your symptoms by phone, get your travel history and listen to your concerns. If the doctor suspects the coronavirus but your symptoms are mild, you’ll likely be advised to self-quarantine at home. The majority of cases are relatively mild, though the disease is more dangerous for older people with underlying medical conditions and people of any age with compromised immune systems. If you are around others, wear a face mask. Avoid sharing personal items, like dishes, and frequently clean countertops, tables and other surfaces.
There is no treatment for covid-19 — there’s nothing like Tamiflu for the flu, for example. Your doctor might write an order for a coronavirus test, but that doesn’t mean it will be honored if your hospital or government health entity decide you don’t fit their guidelines.
People who don’t have a doctor should call their state or local health department to discuss symptoms.
What about going to the ER?
Emergency room doctors are urgently asking those who are worried but well or have mild symptoms to think twice before showing up at the ER. They worry that ERs, which already are seeing increasing numbers of patients, will be flooded, that doctors won’t be able to take care of the seriously ill and that health-care workers might get infected.
“When people recognize disease in community, they get nervous and go to the ER, but that may cause a lot of strain on resources,” said William Jaquis, an emergency medicine doctor at a hospital in Aventura, Fla., and president of the American College of Emergency Physicians.
His group has launched a “Know When to Go” campaign to give patients tips on when they should head to the ER. People who have worsening shortness of breath — like not being able to finish a sentence without taking a breath — should consider going to the ER or even calling 911. Older people with underlying conditions who get sick also should think about getting immediate care.
How do I get tested?
If you have mild symptoms, you probably don’t need to be tested and probably won’t be. If you are sick enough to be hospitalized, you might get tested. If you are in the middle group, it’s still unclear. Contrary to President Trump’s assertion that anyone who wants a test can get it with doctor’s orders, many people have had trouble getting tested.
That’s likely to improve in coming days as more hospital and commercial labs come online and other alternatives, like drive-through testing, pop up.
Some primary care doctors are moving to administer tests for the coronavirus in their offices, but many are reluctant because it carries risks to their patients and themselves. The nose-and-throat swabs can cause patients to cough, potentially infecting the doctors collecting the specimen. The physicians should wear protective equipment, but some practices don’t have it.
For now, “the vast majority of doctors I have spoken to do not have the capacity to do tests on individuals,” said Gary LeRoy, a family physician in Dayton, Ohio, and president of the American Academy of Family Physicians. The organization recently sent Congress a letter complaining their members don’t have basic critical information on issues such as how and when to test their patients and how to deal with a shortage of face masks and gowns.
If you want to get tested, it’s best to call your doctor and find out what’s available.
Are there other places to get tested?
Some hospitals and localities are setting up testing locations away from ERs, clinics and doctors’ offices to minimize the risk of health-care workers and other patients being infected.
Mayo Clinic, for example, just opened a drive-through testing facility. After being screened by phone, people drive through a lane where they provide a cheek swab that is tested for the virus. “Testing in this fashion allows clinic staff to evaluate patients at a location away from the clinic and emergency rooms,” says Jack O’Horo, an infectious disease specialist at Mayo. “This helps protect other patients and staff from potentially coming into contact with the covid-19 virus.”
The White House last Friday said that major retailers had committed to providing parking lot space so that more drive-through facilities can be set up.
Some hospitals are setting up pop-up testing facilities, said Jeremy Faust, an emergency physician at Brigham and Women’s Hospital in Boston. In a recent column in The Washington Post, Faust called for “thousands of pop-up facilities — outdoor assembly lines and tents — to administer the tests immediately. They need not be adjacent to hospitals, and they certainly must not be embedded in emergency rooms.”